Clinical case: Final molar in one day
In this clinical case, Dr Bobby Birdi demonstrates the innovative On1 concept and the benefits of a fully digital workflow.
Single molar tooth replacement is still the hallmark of dental implantology today, and this may continue for many years to come. As a result, numerous implant designs and various restorative solutions have come and gone through the evolution of this type of treatment. Implant therapy in the molar region has benefited from advances in surgical innovation, implant and restorative design, as well as the use of digital technology in treatment planning. This use of digital technology in implant therapy has elevated the precision and predictability of treatment. Nonetheless, it is only the execution of the therapy that has been enhanced overall, and rarely the total treatment time. Even with the use of digital dentistry, the process of molar implant therapy has remained consistent for years. This most often involves implant placement after tooth removal, followed by three to six months of healing, and then an impression (digital or analog), and finally the placement of the final lab-fabricated restoration a few weeks thereafter. Immediate loading of implants in the molar region is not commonly implemented, and even when undertaken, almost always involves the use of a provisional restoration.
However, with the use of digital technology in treatment planning, restorative design, and the execution of computer guided implant surgery it may now be possible to fully synergize surgical and prosthetic aspects of molar implant therapy and truly realize the time benefits that can be offered. This process is started by acquiring and using both CBCT and digital impression technologies. With this digital information, the 3-dimensional location of the final restoration can be completely designed first, and then the surgical anatomy can be properly assessed to precisely and predictably plan the most ideal implant position that will support the final crown. The final screw-retained molar crown may then be fabricated in advance.
This report will describe a clinical case that involves the delivery of a new innovative final pre-fabricated screw-retained implant restoration on the day of implant placement with a one-year follow-up. The benefits of a fully digital workflow will be showcased.
Patient history and profile
A 41-year-old female patient presented in our clinic with a tooth missing at site 36 (Fig. 1). She presented with existing teeth at sites 35 and 37, and an ideal occlusal relationship in the area. Adequate tissue biotype and restorative space was evident clinically as well (Fig. 1). The patient’s medical history was not contributory and she had a better than average dental IQ. The tooth had been missing for approximately six months. Her chief complaint was, “I’d like an implant to replace my missing tooth.”

Fig 1. Pre-Operative radiograph of 36 edentulous site (left). Pre-Operative clinical view of 36 edentulous site (right).
Data acquisition and digital workflow
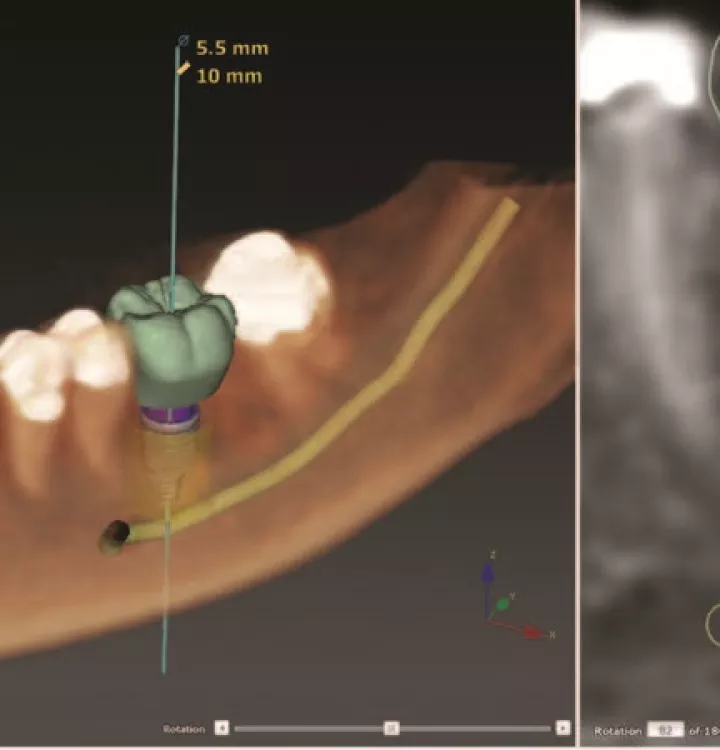
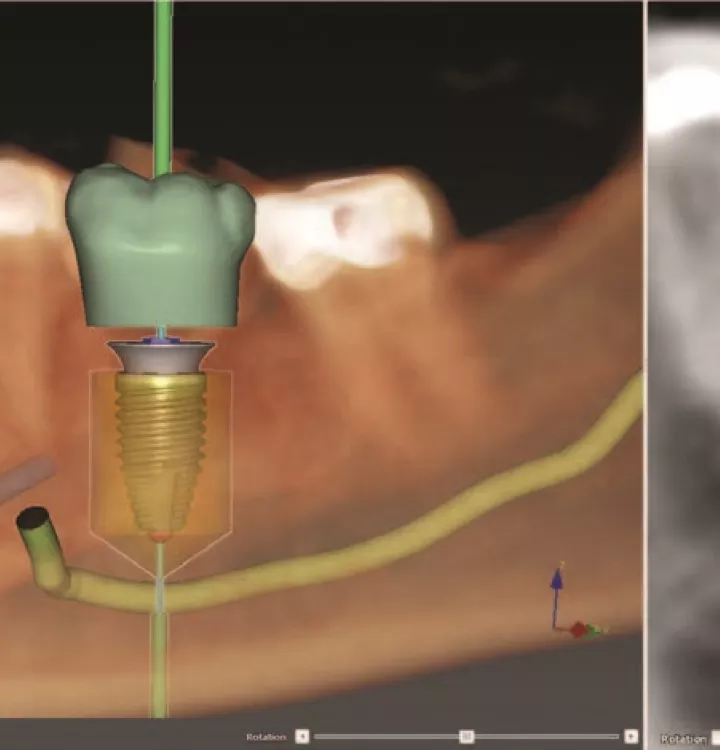
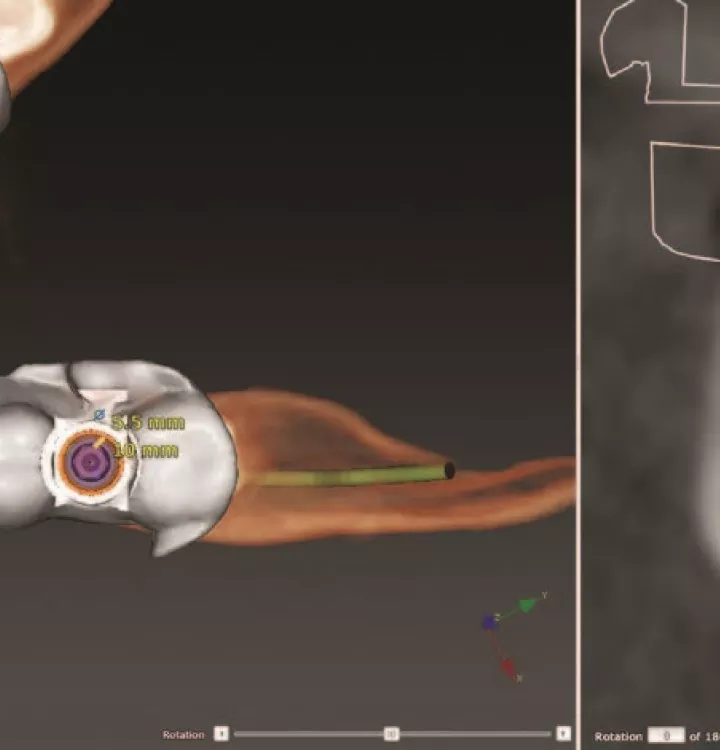
A cone-beam CT scan (ICAT FLX) was completed on the patient as well as a digital impression (3shape Trios 3). These two pieces of digital information were then combined utilizing a software that not only allows for the surgical planning, but the restorative design as well. It is important that the software utilized in and digital implant workflow allows for the full detailed planning of the final restoration as well as the corresponding implant position, in the same software (DTX Studio™ suite) (Fig. 2). The digital workflow can then be fully realized by precisely planning the 3-dimensional position of the final restoration and the technical properties of the final restorative design to allow for ideal and accurate implant placement (Fig. 3). The calculated implant placement in 4 dimensions can then be transferred from the digital workflow to the oral cavity via computer guided surgery. This is the fundamental aspect of the digital workflow and was implemented for this case of molar tooth replacement.
Benefits of wide diameter implant selection
Selecting the correct implant width to be used for a molar site is essential.1 Classically, the width of an implant determined the forces it could tolerate, and the circumference from which the emergence profile would be started. However, with the adoption of platform switching to many implant systems, it is vital to understand that the emergence profile of the restoration commences from the implant connection width and not the actual width of the implant.2 As a result, the presence of a large inequality between the width of the implant and the width of connection results in having to start from a much narrower initial connection circumference, requiring the implant to be placed more apically to allow for the space needed to develop the proper emergence profile. Selecting the appropriate implant connection size that relates best to the mesio-distal and bucco-lingual dimensions of the tooth to be replaced is imperative to long term success.3 Therefore, placing an implant that is larger than 5 mm in diameter (e.g. 5.5 mm) and has a connection size that is also larger than 4 mm in diameter (e.g. 4.4 mm) allows for greater force distribution and tolerances for the molar sites, and furthermore allows for a much more ideal emergence profile to be developed (Fig. 4).
It is also important that the implant connection utilized must continue to have innovations and restorative technological advances occurring to be able to offer contemporary solutions to patients. As a result, the implant selected for this case was one that possessed these attributes (Nobel Biocare Parallel CC WP).
Computer guided implant therapy
The overall digital workflow and surgical planning was transferred from the digital world to the real world via guided surgery4 (Fig. 5). This is the crucial step in the digital workflow. Furthermore, it is only when the decisive implant position is planned based on the ideal position, contours, and design of the final restoration, that the requirement for adjunctive procedures such as osseous and/or soft tissue augmentation can be appropriately assessed. This transfer of the digital plan occurs via the 3D printing of a static surgical guide to be utilized during the guided surgical protocol.
In this clinical case, the surgical guide was printed and fabricated in our dental office/laboratory utilizing a desktop 3D printer (Form 2 Printer – Formlabs) (Fig. 6). The benefits of fully guided implant surgery utilizing a static surgical guide have been demonstrated in the literature for many years. These benefits include increased speed of surgery, minimal invasiveness, and greatly increased accuracy.4,5
The evaluation of the proper seating and fit of the surgical guide is paramount in the accuracy of this procedure. In this clinical case, the fit of the guide was evaluated prior to the surgery. Then a flap was reflected from teeth 35-37 and the 3D printed tooth-borne surgical guide was placed. The series of drills were then utilized to prepare the osteotomy with copious irrigation. Platelet rich fibrin (L-PRF) was utilized in the procedure and was placed into the osteotomy to increase platelet levels in the osteotomy6 (Fig. 7). Then the conical connection implant was placed with an initial stability of over 50 NCm (Fig. 8). A tremendous amount of care was taken to ensure the proper rotational position of the implant was attained as marked on the surgical guide. The reference mark on the surgical guide truly allows for the delivery of the pre-fabricated fully hexed restoration to become a reality. This is a key benefit to a static surgical guide versus dynamic surgical guidance7 (Fig. 9). The surgical guide was then removed and the implant placement position was fully assessed (Fig. 10).
-

Fig 6. 3D printed surgical guide with mark denoting rotational positioning.
-
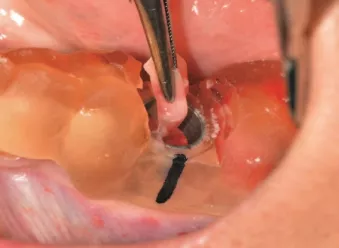
Fig 7. L-PRF being placed into osteotomy prior to implant placement.
-

Fig 8. Molar placement of a NobelParallel™ CC WP implant.
-

Fig 9. Completed placement of NobelParallel™ CC WP implant. Note rotational position.
-
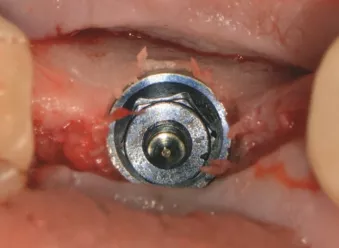
Fig 10. NobelParallel™ CC WP implant in final position and guide removed.
-

Fig 11. On1 Base Xeal (Dr. Bobby Birdi)
On1™ concept perio-prosthetic platform
The implant-abutment connection is by far the most important segment of the overall dental implant complex. The concentration of forces, their release, and the possibility of bacterial colonization all occur in this area. Tissue adherence to components attached to this connection have been demonstrated. As a result, it has been revealed that numerous disruptions to the implant-abutment connection result in tissue damage, irritation, and subsequent bone loss.8-10 Bearing in mind that the switching of components (e.g. healing caps, impression copings, crowns) from within the connection occurs multiple times for each implant case, it is obvious that tissue trauma readily occurs. Moreover, diminished bone loss has been demonstrated when a final abutment is placed into the implant connection on the day of surgical placement and is never removed.8-10 However, the restorative limitations of this are obvious due to angulation and restorative design issues.
As a result, a novel restorative abutment platform was developed to seal off the implant-abutment connection on the day of surgical placement or uncovering and yet permit restorative flexibility (On1™ concept – Nobel Biocare) (Fig. 11).This fully hexed abutment platform was seated and torqued to 35NCm on the day of implant placement for this clinical case at site 36 (Figs. 12 & 13).
-
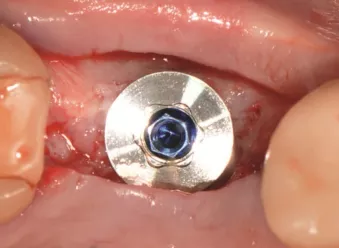
Fig 12. Nobel Biocare WP On1™ Base seated into implant and torqued to 35NCm.
-
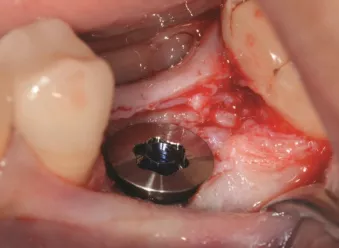
Fig 13. Nobel Biocare WP On1™ Base seated into implant. Note depth of implant placement.
-

Fig 14. Final monolithic zirconia screw-retained hexed crown to seat on Nobel Biocare WP On1™ Base. Pre-fabricated prior to surgery.
-

Fig 15. Final monolithic zirconia screw-retained hexed crown seated Nobel Biocare WP On1™ base and torqued to 35 NCm.
-

Fig 16. Flap advanced and sutured in place around final crown. Access hole filled.
-
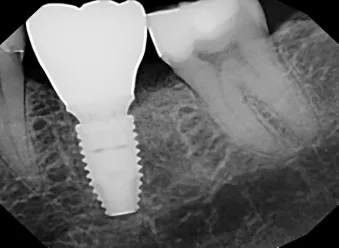
Fig 17. Post-operative radiograph implant placement and delivery of final screw-retained hexed crown on Nobel Biocare WP On1™ Base.
-

Fig 18. Six-week post-operative clinical presentation of the surgical-prosthetic site.
Immediate loading with a CAD-CAM milled final restoration
If the digital workflow has been conducted properly, then the fabrication and delivery of the final restoration should be seamless. In most cases, this begins by taking a digital or conventional final impression after the implant site has healed for three to six months. However, with the advent and utilization of the most current digital technology and workflows, it is possible to deliver the fully hexed final screw-retained monolithic zirconia restoration on the day of surgery. Final molar restorations can be designed to be either screw-retained or cement retained. With recent issues found with retained cement around implant restorations, screw-retained final restorations have become the design of choice.11 The utilization of an immediate implant restoration provides many benefits, with the most important being providing a tooth for the patient on the day of surgery. Up to this point, these restorations have been provisional in nature. But when placed into a controlled environment (teeth present on either side) that is not esthetically demanding, it is very possible to provide a final restoration on the day of implant placement. However, it is essential that to provide this type of service, the implant fixture must be placed at the proper depth and the soft tissue thickness must be adequate.12-13
In this clinical case a fully hexed screw-retained monolithic zirconia restoration (ZirCAD MT Multi-Ivoclar Vivadent) was milled and pre-fabricated in our dental office/laboratory prior to the implant surgery (Fig. 14). It was then delivered at site 36 and torqued to 35NCm on the day of implant placement (Fig. 15). The proximal contacts were ideal and the occlusion needed very little refinement, leaving the tooth in very slight infra-occlusion on maximum intercuspation (verified via shimstock). The flap was then advanced and sutured in place (Fig. 16). The patient was placed on a soft diet for 10 weeks, and she was evaluated at two weeks, six weeks, 12 weeks, and one-year post-operatively. Progressive loading of the area via dietary instructions was completed. The bone levels, tissue levels and overall stability of the area look to be ideal at the latest post-operative appointment. The patient was very happy to have the entire treatment completed in a single surgical-prosthetic appointment (Figs. 17-21).
-

Fig 19. One-year post-operative clinical presentation of the surgical-prosthetic site (Lateral view).
-

Fig 20. One-year post-operative clinical presentation of the surgical-prosthetic site (Occlusal view).
-

Fig 21. One-year post-operative radiograph implant surgical-prosthetic site.
Conclusion
Molar tooth replacement therapy utilizing dental implants and a fully digital workflow has now elevated to new levels. The process can now be predictably completed and allows today’s clinician to deliver a result that is excellent in design, placement, and efficiency. Fully digital implant planning and treatment using highly precise, restoratively driven surgical procedures, not only increases the accuracy and predictability of this treatment, but also allows for the delivery of a final result on the day of implant placement which greatly reduces treatment time. The fully digital final molar implant tooth in one day is a reality today.
Authors
Dr. Bobby Birdi is the co-founder of the Digital Dentistry Institute which is a global learning organization for his fellow dentists, and one of the largest dental educational organizations in North America. He is also founder of the BC Perio Dental Health & Implant Centres in Vancouver, which is one of the largest and most technologically advanced multi-specialty dental centers in Canada. Dr. Farag Edher is a specialist in Prosthodontics. In addition to practicing full time in Vancouver and Coquitlam, Dr. Faraj Edher is a Clinical Assistant Professor and guest lecturer at the University of British Columbia. Dr. Ron Zokol is the founder and co-director of the Pacific Institute for Advanced Dental Education which is an educational institute for dentists. Dr. Sundeep Rawal is co-founder of the Digital Dentistry Institute which is an educational institute for his fellow dentists. His practice out of Orlando, Florida focuses on digital prosthetic treatment and implantology. Dr. Saj Jivraj Education which is an educational institute for dentists.
More to explore
– DTX Studio ™ suite: Digital dentistry software connecting treatment from beginning to end
References
1. Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential stag-ing in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007 Aug;27(4):313-23.
2. Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008 Aug;28(4): 347-55.
3. Rosa AC, da Rosa JC, Dias Pereira LA, et al. Guidelines for selecting the implant diameter during immedi-ate implant placement of a fresh extraction socket: a case series. Int J Periodontics Restorative Dent. 2016;36(3):401-407.
4. Ozan O1, Turkyilmaz I, Ersoy AE, McGlumphy EA, Rosenstiel SF., Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg 2009 Feb;67(2):394-401.
5. Pettersson A, Kero T, Gillot L, Cannas B, Fäldt J, Söderberg R, Näsström K. Accuracy of CAD/CAM-guided surgical template on human cadavers: Part 1. J Prosthet Dent. 2010 Jun;103(6):334-42.
6. Öncü E, Alaaddinoğlu EE. The ef-fect of platelet-rich fibrin on implant stability. Int J Oral Maxillofac Im-plants. 2015 May-Jun;30(3):578-82.
7. Kaewsiri D, Panmekiate S, Sub-balekha K, Mattheos N, Pimkhaokham A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin Oral Implants Res. 2019 Jun;30(6):505-514.
8. Degidi M1, Nardi D, Piattelli A. One abutment at one time: non-removal of an immediate abutment and its effect on bone healing around sub-crestal tapered implants. Clin Oral Implants Res. 2011 Nov;22(11):1303-7.
9. Perrotti V, Zhang D, Liang A, Wang J, Quaranta A. The Effect of One-Abut-ment at One-Time on Marginal Bone Loss Around Implants Placed in Healed Bone: A Systematic Review of Human Studies. Implant Dent. 2019 Aug 1.
10. Canullo L, Pesce P, Tronchi M, Fiorellini J, Amari Y, Penarrocha D. Marginal soft tissue stability around conical abutments inserted with the one abutment-one time protocol after 5 years of prosthetic loading. Clin Implant Dent Relat Res. 2018 Dec;20(6):976-982.
11. Korsch M, Robra BP, Walther W. Cement-associated signs of inflam-mation: retrospective analysis of the effect of excess cement on peri-im-plant tissue. Int J Prosthodont. 2015 Jan-Feb;28(1):11-8.
12. Linkevicius T, Vaitelis J. The ef-fect of zirconia or titanium as abut-ment material on soft peri-implant tissues: a systematic review and meta-analysis. Clin Oral Implants Res. 2015 Sep;26 Suppl 11:139-47.
13. Linkevicius T. The Novel Design of Zirconium Oxide-Based Screw-Retained Restorations, Maximizing Exposure of Zirconia to Soft Peri-implant Tissues: Clinical Report After 3 Years of Follow-up. Int J Periodon-tics Restorative Dent. 2017 J.