“Clinical science and patient satisfaction go hand in hand, and implant dentistry is no exception.”
Nobel Biocare has conducted a multi-center clinical study in three countries with 13 clinicians, looking into the clinical outcomes of implant placement and bone gain after GBR using creos™ xenogain and creos™ xenoprotect in large horizontal defects. The sub analysis results were presented at EAO Congress 2023 in Berlin, where we had the chance to interview Drs. Jonas Lorenz and Marko Magic –study investigators from Germany and Serbia. The focus was on dehiscence, membrane exposure, and their impact on patient-reported outcomes, a topic that has been rarely discussed in the literature.
Dr. Lorenz, Dr. Magic, why did you focus on the impact of dehiscence and membrane exposure on patient satisfaction in the study sub-analysis?
Marko Magic (MM): Patient-reported outcome measures (PROMs), are becoming more important in modern medicine – clinical science and patient satisfaction go hand in hand, and implant dentistry is no exception. I think understanding the PROMs, especially in regenerative dentistry is critical, even if the topic has not received much attention in the past.
Jonas Lorenz (JL): I also think we should focus much more on the patient's perspective, and not only on hard data like bone gain and implant survival. Of course, all the study outcomes are of primary importance for the patient. However, it is necessary to have a deeper understanding of the patient’s perspectives, emotions, and worries especially when it comes to complications and the effects that severe dehiscence could bring about.
What was the ratio of membrane exposure and how were these cases handled?
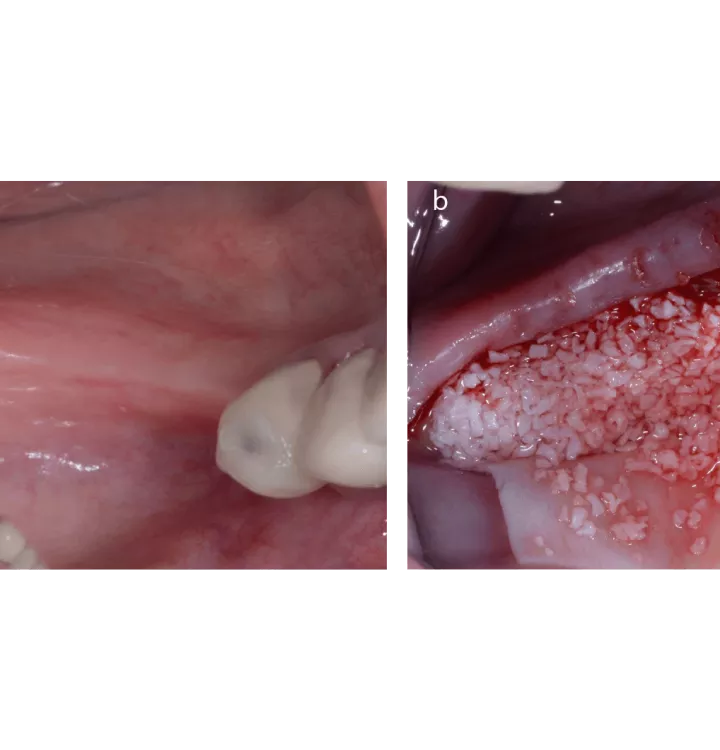
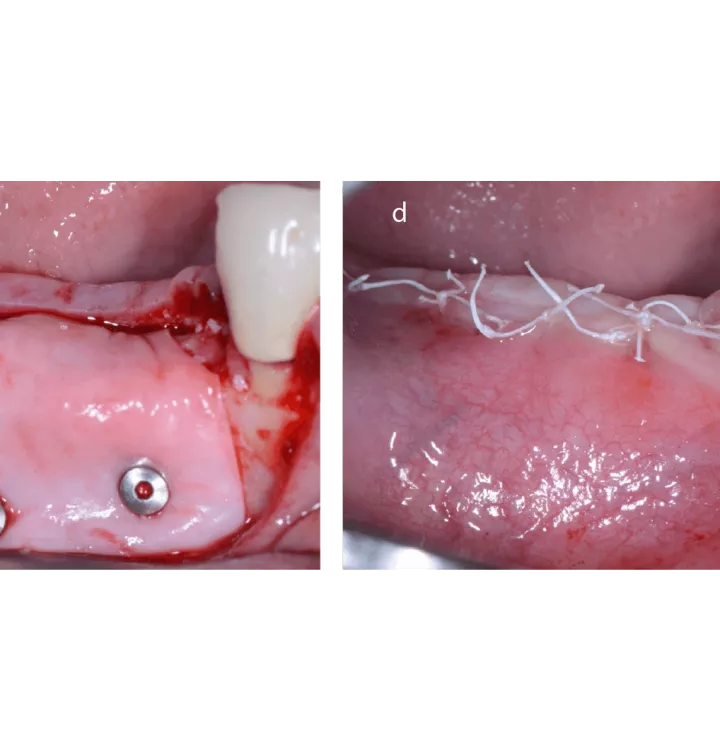
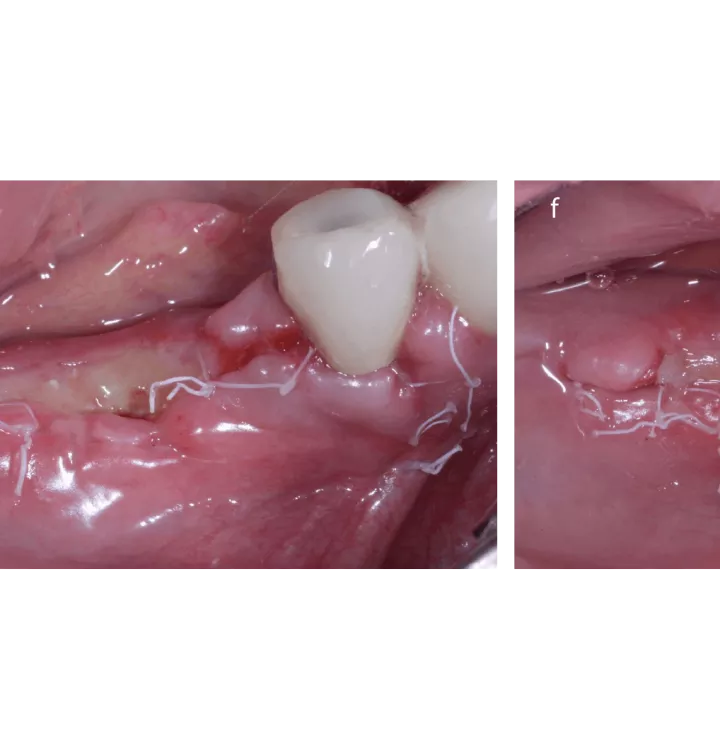
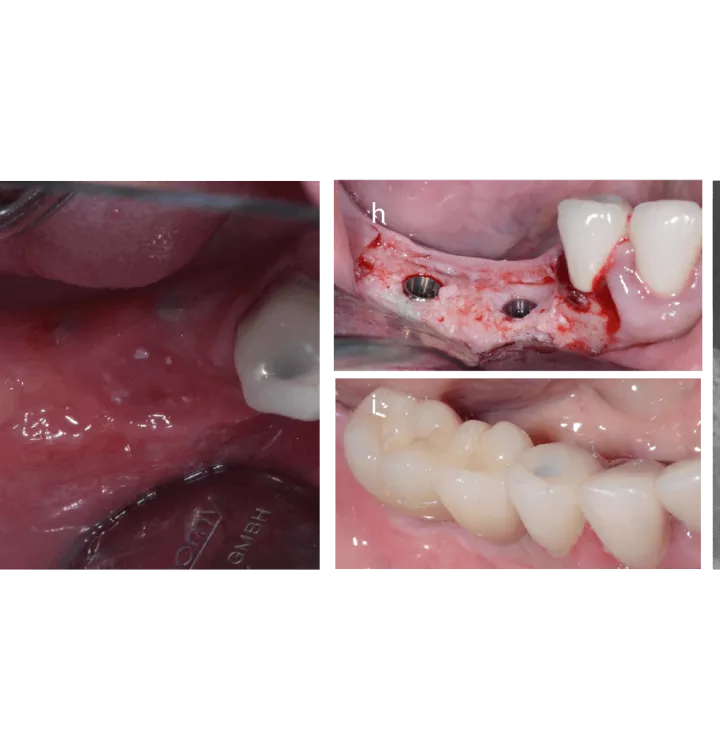
JL: Out of the 45 patients who completed the 8-month healing period follow-up, dehiscence was observed in 9 patients. They were resolved before the 12-week follow-up without any intervention, except in the only two cases of co-occurring membrane exposure (corresponding to 4.3% of the patient population), where one required a secondary stitch and the other a wound cleaning with CHX gel.
MM: We had one case of dehiscence in our center. However, the tissue response was good, it went quite smoothly and the results in terms of bone gain were maybe even better than we expected.
JL: I think it is important to consider dehiscence is rarely a severe adverse event. It can happen often in larger GBRs, depending on clinicians’ surgical skills and experience, and depending on how we can manage the soft tissues. Of course, we should plan carefully how to minimize the risks, or how to manage them when they occur. It is also important not to overreact. The treating clinician should remain calm, and try to treat the dehiscence in a minimally invasive way, e.g. instruct the patient to maintain good oral hygiene and follow up with them more frequently than with a patient without such complications.
How does dehiscence and membrane exposure affect clinical outcomes?
JL: In my experience, there is almost no impact on the clinical results. The results of our sub-analysis in the study show the regeneration of the new bone in the alveolar ridge is not impaired. However, it is not comfortable for the patient if the wound healing is prolonged, and when the patient needs to attend more visits and commit to a more careful hygiene program.
MM: I totally agree that from the bone gain perspective, dehiscence does not impair the results, it rather might be indicative of the initial defect being larger.
The pre-treatment ridge width (RW) in patients with membrane exposure in the study was 2.8 ± 0.7 mm and 3.9 ± 0.8 mm when measured 1 and 3 mm from the crest, respectively, and GBR led to an increase of the RW by 3.2 ± 1.0 mm at 1 mm and 4.1 ± 1.7 mm at 3 mm distance from the crest. And all sites were considered adequate for implant placement and received 17 implants.
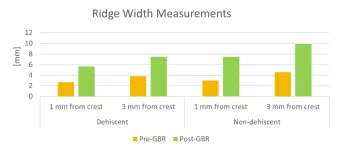
Bone measurements prior to and post GBR in the dehiscent and non-dehiscent group when measured 1 and 3 mm from the top of the crest. The initial defect was greater, and bone gain was smaller in the dehiscence group.
Therefore, it is important that the clinician minimizes intervention, and keeps the patient comfortable. Most of the time, no second surgery or other procedures are necessary, except for increased hygiene maintenance and more frequent check-ups.
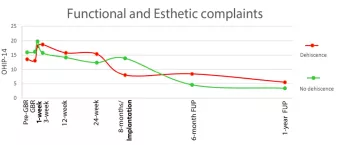
Quality of life (QoL) assessment in patients with vs without dehiscence. OHIP-14 scores range from 0 to 56, with lower scores indicating a better oral health-related QoL. A notable worsening (elevation in scores) in QoL among the general cohort was recorded at 1-week post-GBR and at implant placement, but after both occurrences, patients rebound to the pre-treatment state and beyond. Among the dehiscence subgroup, complaints remained higher than in the general population throughout the 24 weeks of healing.
When do you decide to intervene surgically?
MM: For me, infection is a critical factor. As long as there is no infection, I let the wound heal spontaneously, but I see the patient every second day.
JL: I look at the size of dehiscence, and signs of infection. As long as the dehiscence is limited to the membrane exposure and no sign of inflammation is there, I would only recommend more frequent patient visits. But it is different when the dehiscence is severe, e.g. the bone graft is also exposed, especially when it is not yet integrated and bone particles may move. The more severe it gets, the more likely it warrants the need to intervene. Depending on the wound situation, we might need to remove the membrane and some of the infected materials and additionally administer antibiotics. None of this is comfortable for the patient. This is why I want to highlight again the importance of carefully selecting the biomaterial and planning the surgery to minimize the occurrence of dehiscence and thus patients’ discomfort.
When you use creos™ xenoprotect, which feature of the membrane do you like the most?
JL: For me, first it is the handling properties, and the possibility to shape it during the surgery. But of course, the physiological properties, wound healing, and the regenerative aspect of the material is outstanding as well. MM: I fully agree with you, Jonas. I think that the handling properties of the creos xenoprotect are just wonderful. You can stretch the material and cover big defects. And also, the tissue reaction and the tissue integration of the material are really, really good, even in the case of membrane exposure.
Dr. Laurence, Dr. Magic, thank you so much for sharing your insights.
References
1. Lorenz J, Ghanaati Sh, Aleksic Z, et al. Clinical outcomes after guided bone regeneration with dehiscence during the healing period. Volume34, IssueS27 Special Issue: 30th Annual Scientific Meeting of the European Association for Osseointegration September