Bringing science to the surface: TiUnite study
A newly published meta-analysis evaluating TiUnite implant surface is believed to be the largest such evaluation of a single implant brand ever conducted. Here Prof. Dr. Matthias Karl takes questions on the significance of the study.
A newly published meta-analysis evaluating Nobel Biocare’s TiUnite implant surface1 is believed to be the largest such evaluation of a single implant brand ever conducted. Here, the lead author Prof. Dr. Matthias Karl of Saarland University in Germany takes questions on the significance of the study for researchers, clinicians and patients.
How did you decide which studies to include in the analysis?
Prof. Dr. Karl: “We had strict inclusion criteria. We looked only at prospective clinical studies with at least 20 patients receiving TiUnite implants from the beginning of the study. A minimum of one-year post-loading follow-up was also required. In terms of reporting we had to be able to either derive the accumulative survival rate from the paper or calculate the survival rate based on the data given in the paper.”
Despite the strict inclusion criteria, the study is thought to be the largest analysis of this kind on a single brand of implants. What was the scale of the data examined?
Karl: “It’s certainly the largest such study I’ve seen. We reviewed 106 well-documented prospective clinical studies. To have such a high number of primary studies in a single review is something really unique. In total over 12,000 TiUnite implants were part of the evaluation. This represents a huge database and should be perceived as a real strength for Nobel Biocare, the clinicians using Nobel Biocare implants and their patients. I think it’s really the highest level of evidence we have right now documenting the clinical success of a single implant surface.”
What did you set out to discover within all this data?
Karl: “We did not have any predetermined expectations – this is another strong point of this review in my opinion. It was really, “let’s look and see what we find.” Our aim was not to cherry-pick data, but to conduct an unbiased review of the literature.”
“Another unique feature of the study is that we used implant placement as a base line. Bone remodeling takes place predominantly between implant placement and abutment connection. In many studies it’s only at the prosthetic restoration that the clock starts to run. But by then a certain amount of remodeling has already taken place, it’s more honest to go back and report the implant surgery as the base line and assess the bone levels from then on.”
“We were able to really look at marginal bone level changes from the beginning, from the surgery, for many, many studies, and also looked into biological complications if they had been reported. Of course, we were also looking at peri-implantitis and peri-implant pathology.”
The definition of peri-implantitis is presently a much-debated topic in dental implantology. How did you define it for the purposes of this paper?
Karl: “The definition of peri-implantitis is indeed a hot topic right now. What we have done in the paper is not to over- or underestimate peri-implantitis. If the primary author referenced peri-implantitis or if there was peri-implant inflammation or peri-implant pathology, we counted this as peri-implantitis no matter what. We are well aware that these authors were acting on different scales, but if they used the term ‘peri-implantitis’ or similar we did not question it.”
What were the key findings of your analysis?
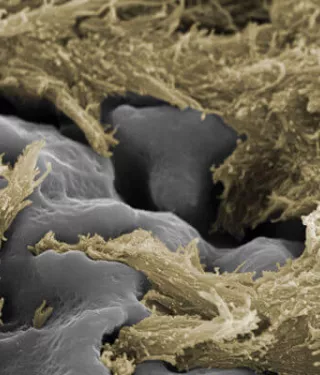
Karl: “For me, the key finding was that TiUnite is a highly reliable implant surface even in very challenging situations. Nobel Biocare has a full range of implant designs with the TiUnite surface and we could not differentiate implant performance between different implant geometries. “In the end you can absolutely say it’s a really great surface. It keeps the implant in place, the longevity is definitely there, it’s proven. The prevalence of peri-implantitis is extremely low. There were no major biological complications and the marginal bone level changes are well within the accepted thresholds for a successful implant.”
How can the findings of your analysis now be used to optimize clinical practice?
Karl: “Clinicians can use the values presented in the paper as a reference. This is the real benefit of such an extensive review. In our own practices we can only see a limited number of patients. What we have here is an analysis of over 12,000 implants spanning a 15-year period. I would say, look at these values and compare it with what you see in your practice. Then you can ask yourself, ‘Where am I in relation to the data and why might that be?’ If you are not seeing the same success, why is this? The findings are a helpful benchmark for modern practice.”
References
1. Karl, M. and Albrektsson, T. Clinical performance of dental implants with a moderately rough (TiUnite) surface: A meta-analysis of prospective clinical studies, Int J Oral Maxillofac Implants 2017;32(4):717-734.