
Experience NobelActive 3.0
Meeting patient needs where space and bone volume are limited.
A widely respected lecturer and dentist, Paul S. Rosen, DMD, MS, is Clinical Associate Professor of Periodontics at the University of Maryland Dental School, and in private practice in Yardley, Pennsylvania, USA.
Dental implants have revolutionized the way that we plan treatment and provide for our patients’ dental needs. The high level of success achieved for dental implants along with their ability to achieve a steady state of health have made them a go-to solution for a wide range of problems.
Yet, despite our desire to meet patient expectations, space and anatomical constraints have at times limited our use of dental implants to replace missing or soon-to-be missing teeth. For example, one of the biggest challenges that clinicians face when placing implants is limited interdental space or inadequate bone volume, which can occur in the maxillary and mandibular anterior region.
In some instances, I have had to advise patients that dental implants were not possible unless I also removed several healthy teeth in addition to the one with the problem to allow for an acceptable final prosthesis that could function with stable health, comfort and esthetics.
Solution at hand
The NobelActive 3.0 mm implant has been a great asset in my practice as it has expanded the treatment options available for my patients.
“Why?” you may ask. In order to maintain adequate bone volume surrounding the dental implant, sometimes the difference between whether or not I will place an implant can be as small as 0.25 mm, and a tapered NobelActive 3.0 mm has the smallest diameter available with a two-piece design.
I want to use a dental implant that is based on a sound foundation. I need to know that the implant is made from commercially pure titanium because it is extremely well tolerated in the human body, has a low incidence rate of adverse biologic reactions, and it provides a surface that is advantageously wettable.
What’s more, I need to feel confident that the implant’s surface has a long-term track record of success, which TiUnite certainly does.
Can the implant provide for good bone height stability after integration? The platform shifting used in the 3.0 design — as in all NobelActive implants — not only allows for this, but also enables excellent emergence profiles for the prosthetics.1-5 Moreover, Martinez-de-Fuentes and colleagues demonstrated improved bone levels during the second year. This is rather important, since we are trying to provide steady state solutions that are esthetically pleasing.
Cases
The first patient illustrates a space challenge and how a 3.0 mm implant can provide a solution (Figure 1a). This 22-year-old male desired a fixed restoration on a dental implant as the bonded fixed prosthesis which he had worn since completing orthodontics had a propensity to loosen and come off at the most inopportune of times.
Revising this area with another resin-bonded prosthesis was also an option, but unacceptable to the patient. The idea of preparing his adjacent teeth for a full coverage fixed partial denture was undesirable due to concerns that endodontics might be needed in the future. A single dental implant was placed with concurrent guided bone regeneration to enhance esthetics at the site of this congenitally missing lateral incisor (Figures 1b–1d).
Following uneventful healing, the implant-supported crown was completed and the patient has been quite happy with the esthetic result (Figures 1e–1g). Moreover, his ability to floss this area and keep the site clean will be important to keep this prosthesis in a steady state of health.
The added benefit of the 3.0 mm implant is that under the right circumstances, it allows for the seemless integration of care, beginning with immediate implant placement and provisionalization that extends up to the delivery of the final crown.
-

Figure 1a. The maxillary right lateral incisor was congenitally missing and space had been left following orthodontics for a dental implant to be placed.
-
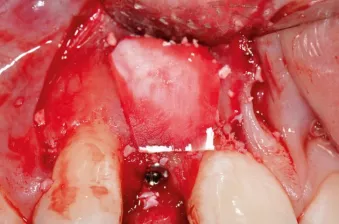
Figure 1b. A 3.0 mm x 13mm NobelActive implant has been placed along with a cover screw.
-

Figure 1c. A bone graft material has been placed where there is a concavity on the facial aspect to enhance esthetics.
-

Figure 1d. A collagen barrier membrane has been placed over the graft.
-

Figure 1e. Close-up view of the final crown cemented in place. (Prosthetic care provided by Howard Rosenthal, DDS, Newtown, Pennsylvania).
-

Figure 1f. View of patient when smiling. The implant-supported crown at the right lateral incisor blends harmoniously with the rest of the dentition.
-

Figure 1g. Periapical radiograph: Limited bone between the implant and the adjacent teeth suggests that the 3.0 mm tapered implant was ideal for this site.
The second patient, a healthy 22-year-old female, was in the process of losing her retained deciduous mandibular right canine due to extensive decay (Images 2a–2b). Space in the area was limited, and treatment was also impacted by the patient’s inability to be present for extended early follow-up; she had taken a summer position in another state.
The sequence of care called for immediate placement and provisionalization of the dental implant if appropriate stability could be achieved. Fortunately, the extraction and surgery went uneventfully with an insertion torque of 35 Ncm allowing for the implant provisionalization (Figures 2c–2d).
The patient was seen at two weeks following extraction to check on early healing and occlusion, and she returned after four months for final impressioning by her restorative dentist. The final crown was delivered two months later (Figures 2e–2f).
In summary, we will continue to be challenged by issues of bone volume and space that require us to have implant sizes and designs that can meet our patients’ needs in these difficult situations.
We need to pursue solutions that are innovative, yet built on sound fundamentals like a commercially pure titanium implant and a time-tested surface, such as TiUnite. The NobelActive 3.0 mm implant represents an outstanding way to expand the options available for missing or soon-to-be lost teeth.
-

Figure 2a. Presurgical view of the retained primary canine on the mandibular right, lateral incisor site. The permanent canine was congenitally missing.
-

Figure 2b. Pretreatment periapical radiograph suggests extensive decay has occurred. There is limited space for a dental implant, dictating the use of the 3.0 mm NobelActive.
-
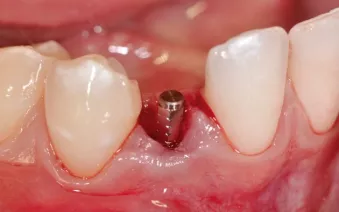
Figure 2c. The tooth has been extracted and a 1.5 mm collar provisional abutment has been inserted onto the implant and torqued to 15 Ncm. A flapless approach has been employed.
-

Figure 2d. Clinical view of the cemented provisional crown which has been kept out of occlusion.
-

Figure 2e. Close-up clinical view of the cemented final crown at six months post-insertion (Prosthetic care provided by Howard Rosen-thal, DDS, Newtown, PA, USA.)
-

Figure 2f. Periapical radiograph obtained six months following the final seating of the crown. The bone level around the implant’s platform has been preserved.
References
Not all featured products may be regulatory cleared/released for sale in all markets. Please contact the local Nobel Biocare sales office for current product assortment and availability.
1. Bardos DI. Titanium and Titanium Alloys. Medical and Dental Materials (Williams D ed.) Pergamon Press 1990, 360-365.
2. Mekayarajjananonth T, Winkler S. Contact angle measurement on dental implant biomaterials. J Oral Implantol. 1999;25(4):230-6.
3. Östman PO, Hellman M, Sennerby L. Ten Years Later. Results from a Prospective Single Centre Clinical Study on 121 Oxidized (TiUnite™) Branemark Implants in 46 Patients. Clin Implant Dent Relat Res. 2012;14:852-860.
4. Glauser R. Implants with an oxidized surface placed predominately in soft bone quality and subjected to immediate occlusal loading: results from a 7-year clinical follow-up..Clin Implant Dent Relat Res. 2013 Jun;15(3):322-31.
5. Martínez-de Fuentes R, Arnhart C, Barlattani A, Goldstein M, Kielbassa AM, Lorenzoni M, Mericske-Stern R, Rompen E, Strub JR. Two-year Follow-up of NobelActive, a Variable-Thread Novel Tapered Implant. J Dent Res 2010;89 (Spec Iss B):4704