The biological environment of immediate placement
In this, the first of a three-part series, Dr. Helms discusses our best current understanding of the biological environment into which implants are placed.
Part one of a three-part series: “Understanding the Biology and Mechanics of Immediate Placement”Working with Liao Wang, Xibo Pei, and Yan Wu at the Stanford University Department of Surgery, Professor Jill A. Helms has been studying what happens around immediately loaded implants. In this, the first of a three-part series, Dr. Helms discusses our best current understanding of the biological environment into which implants are placed.
As times change, regimens change as well. Immediate loading was once considered a biologically untenable treatment. Today we know, however, that it can indeed succeed.
We’ll discuss the immediate implant itself in the next issue of Nobel Biocare News. For now, let’s start with the site in which an immediate implant is placed: an extraction socket.
Trained originally as a periodontist, I rather enjoyed looking at the data related to this subject when we first generated it. The bone-tooth interface is a good place to begin because this will become the bone-implant interface.
Taking a close look at this interface, the first thing one notices is the periodontal ligament (PDL), which is a fibrous tissue, easily verified at high magnification.
In this article, I’m only going to be writing about healthy conditions. I recognize that’s not what one usually faces in the clinic, but that’s what we can study right now in a laboratory, and such a model provides a great deal of insight into the processes that collectively lead to osseointegration.
Because the PDL is a fibrous tissue, it is capable of distorting in response to force. If one subjects a tooth to a lateral force, orthodontic or otherwise, this fibrous tissue elongates on one side of the tooth and compresses on the other. It holds up very well when elongated because it’s fibrous.
The PDL is also capable of compressing—sometimes to the point where it actually “ankylosizes”—but I’ll return to that in a moment.
First, the group studied what happens to the PDL immediately after a tooth is extracted. Using an antibody to a protein called Periostin, which identifies PDL cells, we followed the fate of the PDL in an extraction socket.
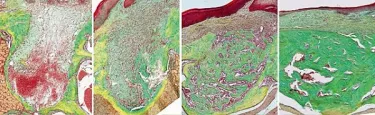
The image to the left shows a very low magnification view of an extraction site—this is just one root—yet the amount of PDL that’s left behind is impressive, to say the least. Something like two-thirds of the socket is surrounded by PDL.
Now I know that a lot of clinicians go in and curette out this tissue— which makes sense if the tissue is diseased—but let me explain what happens to the PDL if the tissue is healthy.
In a case where we haven’t inserted an implant yet, the histology demonstrates that the fibrous PDL tissue that has been left behind curls up. Because the cells still express periostin, however, we know that we are still observing PDL. Sequential imaging over three days post-extraction shows a gradual change in the architecture of the PDL. The cells still express periostin, but in the following days, the PDL turns into bone. It mineralizes.
Our research shows that this is the fate of the PDL in many pathologic conditions—for example when you have ankylosis.
Ankylosis occurs because the PDL is no longer under tension, and it ossifies. For an immediately loaded implant, this is very good news, because the PDL contributes significantly to the amount of bone that forms in the extraction socket.
The series of images are (left to right) from one day, three days, seven days and fourteen days after extraction. One can see how the socket fills in and the PDL is contributing directly to bone healing.
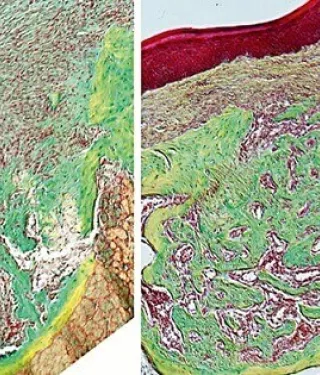
When we ask whether the healing rate of an extraction socket is faster than the rate of bone formation in an osteotomy, the answer is a resounding: “Yes!”
When we compare an extraction socket with an osteotomy, and quantify the amount of bone that forms in each, we repeatedly measure significantly more in the extraction socket than in the osteotomy.
What this tells us, unambiguously, is that extraction sockets heal faster than osteotomies. That means that if you are going to immediately place an implant in an extraction socket, you have an environment very conducive to robust bone formation.
One very important caveat: If the PDL is diseased, the cause of the infection obviously ought to be removed before proceeding with implant placement. Our ongoing research is now focused on understanding how periapical and periodontal disease impacts the immediate placement of implants.