“Soft tissue response has been excellent.” Clinical study of Xeal & TiUltra surfaces, explained
An active member of the Italian Academy of Prosthetic Dentistry, Dr. Giacomo Fabbri lectures internationally on prosthodontics and has published numerous articles in peer-reviewed journals while maintaining a private practice in Cattolica, Italy. One of the first clinicians to use Xeal abutments and TiUltra implants – designed to optimize tissue integration from abutment to the implant apex – he has been leading a clinical study to monitor the treatment outcomes with these new surfaces. With the one-year results presented at the Academy of Osseointegration 2022 Annual Meeting, we interviewed Dr. Fabbri to discuss his findings
Can you briefly explain the design and purpose of this study?
Surface chemistry and topography are key factors in osseointegration and the Mucointegration™ process. Nobel Biocare updated their application of anodization – possibly the most studied and well-proven implant surface technology – and we decided to monitor and evaluate the clinical performance of TiUltra implants and On1 Xeal abutments over three-years of function.
It is a prospective, single-center study, which has enrolled patients that required one single-tooth replacement in the premolar or molar area in either jaw. Evaluation includes implant survival and success, marginal bone remodeling, and soft tissue health assessments.
What treatment protocol is being followed?
The variable thread tapered implant, NobelActive TiUltra, was placed in healed sites, and an anodized abutment base, On1 Base Xeal, was immediately attached to the implant and a healing cap connected to it. The final prosthesis was placed about four months later. The sites include both premolar and molar, and maxilla and mandible.
We can now see the results of one-year follow-up. What are your key findings?
The crucial aspect is that in all the cases, we observed an improvement of bone and soft tissue integration at 1-year follow-up. Soft tissue response has been excellent. There is increased keratinized mucosa presence and height, from 3.7 ± 0.9 mm at implant insertion to 4.0 ±1.0 mm at one year.
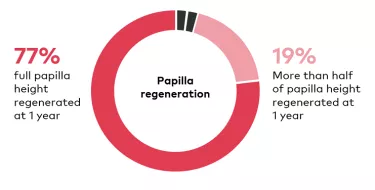
We also see robust papilla maturation. Based on the Jemt papilla score, seventy-seven per cent had optimal soft tissue contour at one year, followed by nineteen per cent having at least half of papilla height regenerated.
Soft tissue health is clearly extremely positive. What about bone response?
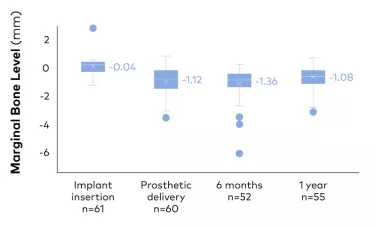
Again, the results are very promising. From prosthetic delivery to one-year follow-up after expected post-insertion bone remodeling, there are stable marginal bone levels of +0.04 ±0.76 mm. In many cases, in particular where the remodeling following implant insertion was higher, an important bone gain one-year after the prosthetic delivery was also observed, with almost complete recovery of the defect. Overall, we see stable marginal bone levels from prosthetic delivery to one-year follow-up, after the expected remodeling following implant insertion.
When clinicians see these study findings, what should be their key takeaway? How is it relevant to daily practice?
The key point here is that if we want to protect and preserve the bone, first we need to optimize the soft tissue healing and integration. The soft tissue integration represents a crucial aspect for an ideal prosthetic integration and, at the same time, is the first defense barrier for the surrounding bone.

You recently authored the eBook, A Comprehensive Approach to Plan and Design the Emergence Profile Around Dental Implants. How does surface affect emergence profile?
The emergence profile of each implant includes a bone interface and a soft tissue interface, and to have a tailored surface in each area represents a great achievement in order to get best integration at every level. This aspect has a paramount value also in a long-term perspective in order to improve the longevity of our restorations.
How does implant choice affect emergence profile?
The implant and abutment selection, considering morphology, size, connection design, represent important factors for planning an ideal emergence profile in each clinical situation. In addition, the prosthetic components, including all the possible restorative solutions play a significant role in this.
What are the biggest challenges in achieving an adequate emergence profile?
The key challenge is a correct 3-dimensional implant placement in relation to the bone anatomy, the prosthetic wax-up and the final anticipated soft tissue contour. This is the first point for the success. Fortunately today’s digital technology, including static and dynamic guided surgery, allows implant placement in a prosthetically- and biologically-driven approach.