Early dental implant failure: 4 tips on lowering risks to osseointegration
Oral surgeon Dr. Annette Felderhoff-Fischer offers tips on avoiding early risks to osseointegration, and how the Nobel Biocare N1™ system can help.

Dental implants have become an extremely successful therapy in recent years, both in partially edentulous and edentulous cases.1,2,3,4 In order to continue and even improve this success for as many patients as possible, there are some basic considerations that should be included in the procedure, starting with the indication and planning. Based on my own clinical experience, and the training I have been involved in and provided over the past 20 years, I have some advice on optimizing your chance for success from the start.
- 1. Carry out detailed implant treatment planning
- 2. Assess bone quality before implant site preparation
- 3. Implant torque and primary stability
- 4. Passive fit
- 5. Nobel Biocare N1™ dental implant system
- 5.1. Assessing bone quality: How can site preparation with the Nobel Biocare N1…
- 5.2. Why have I chosen to use the N1™ implant system?
Carry out detailed implant treatment planning
Careful patient selection and well-founded planning are essential. Before each procedure, always check whether the patient is suitable for implant treatment based on their general medical history, periodontal condition and oral hygiene.
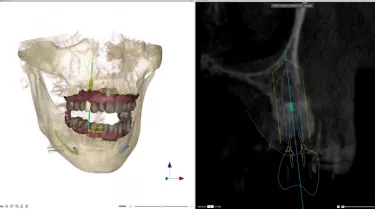
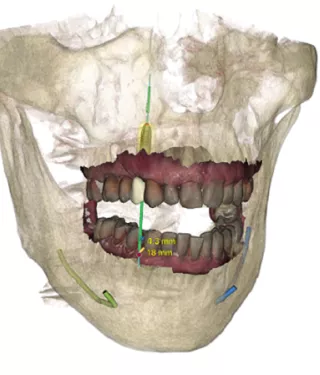
In addition, I strongly recommend diagnosis and planning of the procedure with 3D imaging and planning software. Bone volume can be analyzed with CBCT and allow for implant selection in terms of length and diameter preoperatively, taking into account anatomical risk structures. Furthermore, the planning takes the tissue management and the final prostheses into consideration, allowing you to optimize the planned implant placement based on the final treatment outcome desired.
Assess bone quality before implant site preparation
Implant site preparation should aim to keep bone trauma to a minimum and assist primary stability. As such, site preparation requires knowledge of the bone quality.
A big challenge at this stage is a degree of guesswork that this entails. While the experienced implantologist might “feel” the bone quality with the first drill, if you are not an implant specialist or have less experience in implant treatment, you should regularly attend hands-on training to improve this ability, and I particularly recommend attending cadaver training courses.
This knowledge is important because the drilling protocol is adapted depending on bone quality, to not over- or under-size the implant site. Conventional site preparation requires the use of multiple drills with different diameters which, together with irrigation, cause trauma to the surrounding alveolar bone5: a so-called “zone of death”. If the trauma is too great – which can occur especially in a lower jaw with predominantly cortical bone (bone quality I) – osseointegration might be impeded. If the trauma is mainly around the platform, vertical resorption can occur. Excessive preparation of predominantly cancellous bone (bone quality IV) also leads to a lack of primary stability of the implant, and potentially early implant loss.6
Implant torque and primary stability
The next step is the selection of the implant itself, which is again influenced by bone quality and the preparation of the implant site. The choice of implant (geometry, diameter, platform) and implant site preparation (underpreparation of the osteotomy) influences primary stability and is therefore an important factor for osseointegration.7 A much-discussed figure is the torque value. High torque values are often viewed as positive for immediate loading. However, overtightening may damage or fracture the implant and could cause necrosis of the bone site and early dental implant failure.6
A 35 Ncm value is often recommended as standard, however I personally do not see the torque values of the individual implant systems as being comparable with one another, as the individual geometry of an implant causes different reactions in the bone. The implant manufacturer provides guidance on maximum torque values, and you should follow this.
Passive fit
A gap-free and tension-free connection between the implant and the superstructure, and regular follow-ups soon after treatment, alongside stable oral hygiene are important for success.
You should aim for a gap-free and tension-free prosthetic reconstruction, both with immediate loading and with delayed restorations. If this is not the case, vertical bone loss or screw loosening occurs and, as a result, peri-implant complications. Particularly with connections featuring a deep cone, taking an impression of multiple implants carries the risks of inaccuracies and tension, which should be taken into account when planning a screw-retained restoration. If screw loosening occurs, the restoration must be removed, the cause determined, and a new original screw of the implant system inserted again.
Nobel Biocare N1™ dental implant system
Assessing bone quality: How can site preparation with the Nobel Biocare N1™ implant system help?
One of the critical factors in treatment planning and site preparation is the assessment of bone quality. Regardless of pre-surgical investigation, clinical decisions are often dependent upon tactile and visual judgement during surgery and, unfortunately, this is a skill that can only be acquired through experience.8
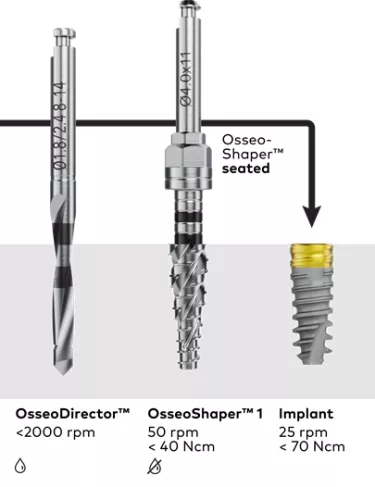
This is one of the drawbacks that the Nobel Biocare N1™ surgical protocol has been designed to address. After creating a pilot osteotomy with the OsseoDirector™, the OsseoShaper™ site preparation instrument ‘shapes’ the osteotomy at low speed and matches the shape of a co-packed implant. This protocol provides a gauge to indicate bone quality, minimizing guesswork and decision making. If the OsseoShaper 1 instrument can be fully seated at the planned depth, the implant can then be placed. In a survey of clinicians, the implant could be placed after just these two steps in the majority of cases – 87.8%.*
If OsseoShaper 1 does not reach the planned implant depth before achieving a torque of 40 Ncm, the OsseoShaper 2 instrument can be used. If the same also occurs with the OsseoShaper 2 instrument, then the N1 Twist Drill can be used.
Not only does this assist clinical decision making, but because the instrument operates at low speed and without irrigation, it has been shown to create less trauma, leading to earlier bone formation compared to conventional high-speed techniques.5 It has been designed to preserve vital bone chips in the osteotomy to promote fast osseointegration.
*303 implants in 160 patients using CE-marked pre-launch portfolio. April 2019 – May 2020. Data on file.
Why have I chosen to use the N1™ implant system?
As an oral surgeon, I am fascinated by the biological benefits of gentle implant site preparation based on osseointegration research by the team led by Prof. Jill Helms. As well as knowing that bone experiences less biological trauma compared to conventional techniques, I also find the clinical procedure much simpler, and, based on patients’ feedback, that the reduced noise and vibration makes it more comfortable for them. Coming from navigated implantology in which the drills are guided through sleeves, I also like minimizing guesswork when not using guides. The OsseoDirector indicates direction, and the OsseoShaper and implant follow. In most cases, I can place the implant in just these three steps. I like the simplicity, and the benefits it brings to my patients.
References
1. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10-16-year follow-up of non-submerged dental implants Clin Oral Implants Res; 2010 Jul;21(7):772
Read on PubMed
2. Wennerberg , Alrektsson T, Chracanovic B. Long-term clinical outcome of implants with different surface modification. Eur J Oral Implantol 2018;11(Suppl 1): S123–S136
Read on PubMed
3. Karl M, Albrektsson T. Clinical performance of dental implants with a moderately rough (TiUnite) surface: a meta-analysis of prospective clinical studies. Int J Oral Maxillofac Implants 2017;32(4):717–734.
Read on PubMed
4. Malo P, de Araujo Nobre M, Lopes A, et al. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin Implant Dent Relat Res 2019;21(4):565-577.
Read on PubMed
5. Chen, C.-H.; Coyac, B.R.; Arioka, M.; Leahy, B.; Tulu, U.S.; Aghvami, M.; Holst, S.; Hoffmann, W.; Quarry, A.; Bahat, O.; Salmon, B.; Brunski, J.B.; Helms, J.A. A Novel Osteotomy Preparation Technique to Preserve Implant Site Viability and Enhance Osteogenesis. J Clin Med. 2019 Feb 1;8(2):170
Read on PubMed
6. Ikar M, Grobecker-Karl T, Karl M, Steiner C. Mechanical stress during implant surgery and its effects on marginal bone: a literature review Quintessence Int. 2020;51(2):142-150
Read on PubMed
7. Fawad Javed, George E. Romanos, The role of primary stability for successful immediate loading of dental implants. A literature review, J Dent., 2010 Aug;38(8):612-20
Read on PubMed
8. Velikov S, Susin C, Heuberger P, Irastorza-Landa A. A New Site Preparation Protocol That Supports Bone Quality Evaluation and Provides Predictable Implant Insertion Torque. J Clin Med. 2020;9(2).
Read on PubMed
GMT73942 © Nobel Biocare Services AG, 2021. All rights reserved.
Nobel Biocare, the Nobel Biocare logotype and all other trademarks are, if nothing else is stated or is evident from the context in a certain case, trademarks of Nobel Biocare. Please refer to nobelbiocare.com/trademarks for more information. Product images are not necessarily to scale. All product images are for illustration purposes only and may not be an exact representation of the product.
Disclaimer: Some products may not be regulatory cleared/released for sale in all markets. Please contact the local Nobel Biocare sales office for current product assortment and availability. See Instructions For Use for full prescribing information, including indications, contraindications, warnings and precautions.