“Digital technologies cover 80 to 90 per cent of the entire treatment”

Following last year’s fully-booked three-day course, the upcoming Masterclass in Esthetic Implant and Restorative Dentistry will be held at the University of Zurich, November 10-12. One of the most comprehensive courses in advanced implant treatment, featuring live surgeries, and hands-on sessions, participants will gain 21 CE credits. We spoke with Prof Daniel Thoma who is co-organizing the course in collaboration with Prof Ronald Jung and the team from the Clinic of Dentistry.
What are the aspirations of this year’s course?
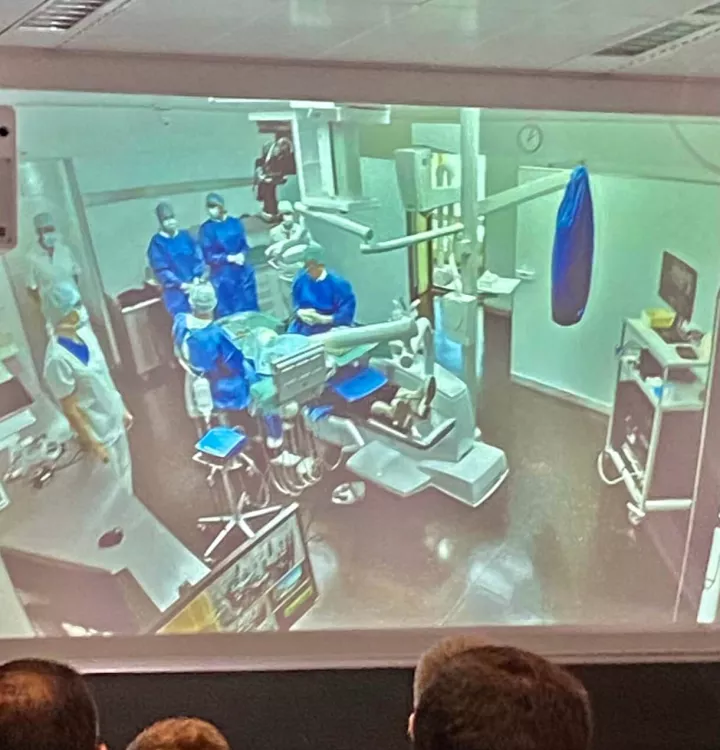
The Masterclass shows the entire therapy concept from first examination to final restoration, and of course the long-term outcomes. So it’s going be a mix of lectures, hands-on exercises, and two live surgeries. The first one is an implant placement in conjunction with GBR in the esthetic zone and the second one handles soft tissue on the dental implant side. I think this makes the Masterclass really different from other courses because we have excellent facilities that allow us to stream live the surgical events and also allow participants to ask questions directly during the surgery.
You have run the Masterclass for a few years now, what are the participants’ main motivations to join? What have they liked most?
I think what participants really like is the small-group experience. Our entire team stays with them for the whole three days. We all have the feeling of being part of a family. This proximity also makes it way easier to answer questions that participants may have, not only related to the surgical interventions and lectures, but more generally to their clinical work. We always change the topics of the program according to new scientific data and because the daily clinical work is changing. So we provide participants with the latest updates.
Live surgeries this year are focused on soft and hard tissue management in the esthetic zone. Can you tell us why these procedures are essential for the final esthetic outcome?
When looking at the type of research that is currently being performed, esthetics are really important to patients. Soft tissue augmentation procedures are the basis for providing the best esthetic outcome and they are also essential to maintain peri-implant health over the long run. We provide the participants with the whole workflow, which really makes a difference. Traditionally you just see some workflows on a 2-minute video, but here you have surgery which probably takes about an hour. So you actually get the entire surgery and not only the highlights.
How do you assess success in terms of esthetic outcome, both from your and the patient’s perspective?
That’s an extremely difficult question. When you look into research, there are a lot of indices and measurements on how we assess esthetics. The most well-known one is the pink esthetic score (PES). There has actually been some recent scientific evidence that demonstrates that there is somehow a discrepancy between professionally assessed outcomes, and patient-reported outcomes. So, what is the success of the treatment? I guess the success of the treatment is a happy patient and the success of the treatment may not be a patient where we have the highest pink esthetic score, because very often the patient can’t even tell the difference. Today we have changed the way we provide patients with dental care based on studies that take into account patient-reported outcome measures.
How do you manage teamwork in the Clinic of Reconstructive Dentistry at every step, from the initial consultation to surgery and patient aftercare?
The team approach is important, not only for the outcome, but predominantly for the patient, especially whenever we talk about implants, or complex restorations. Patients come to see us many times and, at the end, they really like having the same dental assistant and also the dental technician involved already from the beginning with the clinician. Patients tend to be a bit afraid of treatments and they associate that usually with the clinician. So having a team makes them feel usually way more comfortable.
Treatment planning should be simple and predictable, to what extent does digital technology help fulfilling this goal?
We always think that digital technologies are a bit far away and that’s something of the future. But at the end I would make a guess that digital technologies cover 80 to 90% of the entire treatment. Just one example – the mockups in most cases are made fully digital today. Digital technologies really help us to simplify treatment because they take away some of the basic decisions. For example, let’s talk about placing an implant with guided surgery. This actually takes away a lot of the stress during surgery because as a clinician you already know even before the surgical intervention exactly how much bone you have, what difficulties you could observe during surgery. So I think the stress level is much lower using these technologies.
Tell us something about the choice of reconstructive materials. Which technical and biological criteria should be taken into account?
We try to have an evidence-based approach. We have seen some evolution in the past couple of years. I remember maybe 10 years ago we were able to provide the patient with a lot of different materials. And then, thanks to science, we observed that some of these materials for restorations would have a lot of complications and we had to adapt our clinical workflow and the materials we use on a daily basis. I think there has been a clear shift also thanks to digital technologies. For instance, PFM restorations are hardly used anymore, and that’s thanks to science. Now we can offer hybrid solutions, meaning that you have for example a titanium intermediate abutment and then on top you have a digitally designed and milled restoration most often being zirconia. The accuracy and the precision of these new technologies are at an extremely high level. During these three days we will be also focusing on the choice of the materials and the respective biological and technical complications that we have to observe.
As an academic, how do you see the curriculum evolving in the field of implantology? Which set of skills and knowledge should be promoted among dental students?
We have seen already a clear shift and the curriculum is changing and being adapted all the time. When we look back, maybe 15 years ago, implants were predominately provided by specialists, but that is gone. Today, when you open a private practice as a general dentist, you need to be able to place dental implants. You may not feel comfortable to place implants in the esthetic zone or for very complex cases, but as a basis, you need to be able to provide patients with implants. So we also had to adapt the curriculum that we offer and offer more knowledge, and more skills to students so that they know that implants are an important tool to provide patients with the best therapy.